Cardiovascular Diseases
Arrhythmias
Metabolic
abnormalities should always be ruled out before performing Holter monitor
studies or committing to long-term antiarrhythmic therapy (e.g.,
hypokalemia, hypomagnesemia, anemia, hypoxemia, hypo- or hyperthyroidism).
Arteriovenous
Fistulas, Angiomatous, Congenital
Platelet count may be decreased.
Behēet's
Syndrome
- (Systemic
vasculitis involving arteries and veins characterized by triad of
recurrent aphthous ulcers of mouth and genitalia, and relapsing
panuveitis.)
- No definitive laboratory
tests
- Laboratory findings due
to involvement of various organ systems, e.g.,
- Large vessel occlusion
(e.g., aneurysms, arthritis, meningitis) Skin
lesions
Churg-Strauss
Syndrome (Allergic Granulomatosis and Angiitis)
- Biopsy showing granulocytes around an arteriole and venule establishes the
diagnosis.1
- ESR is high.
- WBC count is increased.
- Eosinophilia is usual and
seems to correlate with disease activity.
- Serum IgE is often
increased.
- p-ANCA is found in ≤60%
of patients. c-ANCA is rare.
Cor
Pulmonale
- Secondary polycythemia
- Increased blood CO
when cor pulmonale is secondary to chest deformities or pulmonary
emphysema
- Laboratory findings of
the primary lung disease (e.g., chronic bronchitis and emphysema, multiple
small pulmonary emboli, pulmonary schistosomiasis)
Coronary
Heart Disease (CHD)
- Increased risk factors
- Increased serum total
and LDL cholesterol, decreased HDL cholesterol and various ratios (see Chapter 12).
- Recent reports suggest
that apo A-I and apo B may be better discriminators of CHD than
cholesterol, and low ratio of apo A-I to apo B may be best predictor.
(Variation in methodology and lack of interlaboratory standardization
makes this difficult to evaluate at present.)
P.114
- Atherogenic index
(combination of ratio of LDL to HDL × apo B with ratio of apo B to apo
A-I) =

- Increased serum
homocysteine >15.9 µmol/L (normal = 5-15 µmol/L) triples risk of AMI.
Each increase of 5 µmol/L increases risk equivalent to increased
cholesterol of 20 mg/dL. Increase may be due to vitamin B deficiency or
genetic deficiency of methylene-tetrahydrofolate reductase enzyme.
Increased in end-stage renal disease dialysis patients and in
hypothyroidism, certain drug therapies (e.g., methotrexate [transient],
phenytoin and carbamazepine [mild], theophylline, nitrous oxide), cigarette
smoking.
- Low plasma vitamin B and folate levels are each independent risk factors for cor 717d36h onary
artery disease.
- Increased serum
triglyceride level is a risk factor but may not be independent of other
factors.
- Clinical evidence of CHD
or atherosclerosis in patient <age 40, family history of premature
CHD, hypertension, male gender, smoking.
- Syndrome X: insulin
resistance, low HDL level, high level of very low density lipoproteins
(VLDLs) and triglycerides.
- Various abnormalities of
blood clotting mechanisms (e.g., fibrinogen, factor VII, antithrombin
III, phospholipid antibodies, protein C, protein S).
- Lipoprotein
electrophoresis (see Table 13-6) shows a specific
abnormal pattern in <2% of Americans (usually types II, IV). Chief
purpose of test is to identify rare familial disorders (I, III, V) to
anticipate problems in children.
- Lipoprotein
electrophoresis may be indicated if serum triglyceride level is >300
mg/dL, fasting serum is lipemic, or hyperglycemia, significant glycosuria,
impaired glucose tolerance, or increased serum uric acid (>8.5 mg/dL)
is present.
- Perform laboratory tests
to rule out diabetes mellitus, liver disease, nephrotic syndrome,
dysproteinemias, hypothyroidism.
Endocarditis,
Bacterial
- Blood culture is positive in 80-90% of patients. Streptococcus
viridans causes 40-50% of cases; Staphylococcus
aureus, 15-20%; Streptococcus pneumoniae,
5%; and Enterococcus, 5-10%. Other causes may be
gram-negative bacteria (~10% of cases; e.g., Escherichia
coli, Pseudomonas aeruginosa, Klebsiella,
Proteus) and fungi (e.g., Candida, Histoplasma,
Cryptococcus). Bartonella has been
reported to cause 3% of cases, which may be culture negative.
- In drug addicts, S. aureus
causes 50-60% of cases and ~80% of tricuspid infections; gram-negative
bacteria cause 10-15% of cases; cases due to polymicrobial and unusual
organisms appear to be increasing. ≤75% of patients may be HIV
positive.
- Proper
blood cultures require adequate volume of blood, at least five cultures
taken during a period of several days with temperature of 101°F or more
(preferably when highest), anaerobic as well as aerobic growth, variety of
enriched media, prompt incubation, prolonged observation (growth is usual
in 1-4 days but may require 2-3 wks). Beware of negative culture
due to recent antibiotic therapy. Beware of transient bacteremia after
dental procedures, tonsillectomy, etc., which does not represent bacterial
endocarditis (in these cases, streptococci usually grow only in fluid
media; in bacterial endocarditis, many colonies also occur on solid
media). Blood culture is also negative in bacterial endocarditis due to Rickettsia burnetii, but phase 1 complement fixation
test is positive.
- Positive blood cultures may be more difficult to obtain in prosthetic valve
endocarditis (due to unusual and fastidious organisms), right-sided
endocarditis, uremia, and long-standing endocarditis. A single positive
culture must be interpreted with extreme caution. Aside from the
exceptions noted in this paragraph, the diagnosis should be based on two
or more cultures positive for the same organism.
- Serum bactericidal test
measures ability of serial dilutions of patient's serum to sterilize a
standardized inoculum of patient's infecting organisms; it is sometimes
useful to demonstrate inadequate antibiotic levels or to avoid unnecessary
drug toxicity.
P.115
- Progressive normochromic
normocytic anemia is a characteristic feature; in 10% of patients, Hb
level is <7 gm/dL. Rarely there is a hemolytic anemia with a positive
Coombs' test. Serum iron is decreased. Bone marrow contains abundant
hemosiderin.
- WBC is normal in ~50% of
patients and elevated ≤15,000/cu mm in the rest, with 65-86%
neutrophils. Higher WBC indicates presence of a complication (e.g.,
cerebral, pulmonary). Occasionally leukopenia is present. Monocytosis may
be pronounced. Large macrophages may occur in peripheral blood.
- Platelet count is usually
normal, but occasionally it is decreased; rarely purpura occurs.
- Serum proteins are
altered, with an increase in gamma globulin; therefore positive ESR and
tests for cryoglobulins, RF, etc., are found. Often a direct correlation
is seen between ESR and course and severity of disease.
- Hematuria (usually
microscopic) occurs at some stage in many patients due to glomerulitis,
renal infarct, or focal embolic GN.
- Albuminuria is almost
invariably present, even without these complications. Renal insufficiency
with azotemia and fixed specific gravity is infrequent now.
- Nephrotic syndrome is
rare.
- CSF findings in various
complications, meningitis, brain abscess
- Laboratory findings due
to underlying or predisposing diseases or complications
- Rheumatic heart disease.
- Congenital heart
disease.
- Infection of
genitourinary system.
- Congestive heart
failure.
- Bacterial endocarditis
occurs in ≤4% of patients with prosthetic valves.
- Other.
Giant
Cell Arteritis (GCA)
- (Systemic
panarteritis of medium-sized elastic arteries)
- Biopsy of involved segment of temporal artery is diagnostic,1 but negative biopsy does
not exclude GCA because of skip lesions. Therefore, surgeon should remove
at least 20 mm of artery, paraffin sections of which must be examined at
multiple levels. Biopsy findings remain positive for at least 7-14 days
after onset of therapy.
- Classic triad of increased ESR (≥50 mm/hr),1 anemia, increased serum
ALP is strongly suggestive of GCA.
- Mild to moderate
normocytic normochromic anemia is present in 20-50% of cases and is rough
indicator of degree of inflammation.
- ESR is markedly increased
in virtually all patients (97%); average Westergren = 107. A normal ESR
excludes the diagnosis when little clinical evidence exists for temporal
arteritis. CRP test has equal sensitivity.
- Serum ALP is slightly
increased in ~25% of patients.
- WBC is usually normal or
slightly increased with shift to the left.
- Platelet count may be
nonspecifically increased.
- Serum protein
electrophoresis may show increased gamma globulins. Rouleaux may occur.
- Serum CK is normal.
- Laboratory findings
reflect specific organ involvement.
- Kidney (e.g., GN).
- CNS (e.g., intracerebral
artery involvement, which may cause increased CSF protein; stroke;
mononeuritis of brachial plexus).
- Heart and great vessels
(e.g., myocardial infarction, aortic dissection, Raynaud's disease).
- Mild liver function abnormalities
in 20-35% of patients.
- SIADH.
- Microangiopathic
hemolytic anemia.
- Polymyalgia rheumatica
is presenting symptom in one-third of patients and ultimately develops in
50-90% of cases.
Heart
Failure
- Renal changes:
- Slight albuminuria
(<1 gm/day) is common.
P.116
- Isolated RBCs and WBCs,
hyaline, and (sometimes) granular casts.
- Urine is concentrated,
with specific gravity >1.020.
- Phenolsulfonphthalein
(PSP) excretion and urea clearance are usually depressed.
- Moderate azotemia (BUN
usually <60 mg/dL) is evident with severe oliguria; may increase with
vigorous diuresis. (Primary renal disease is indicated
by proportionate increase in serum creatinine and low specific gravity of
urine despite oliguria.)
- Oliguria is a
characteristic feature of right-sided failure.
- ESR may be decreased
because of decreased serum fibrinogen.
- Plasma volume is
increased. Serum albumin and total protein are decreased, with increased
gamma globulin. Hct is slightly decreased, but RBC mass may be increased.
- Plasma sodium and chloride
tend to fall but may be normal before treatment. Urine sodium is
decreased. Total body sodium is markedly increased and potassium is
decreased. Plasma potassium is usually normal or slightly increased
(because of shift from intracellular location); it may be somewhat reduced
with hypochloremic alkalosis due to some diuretics.
- Liver
function changes
- Laboratory findings due
to underlying disease (e.g., rheumatic fever, viral myocarditis, bacterial
endocarditis, chronic severe anemia, hypertension, hyperthyroidism,
Hurler's syndrome).
- Acidosis (reduced blood
pH) occurs when renal insufficiency is
associated or CO retention exists due to
pulmonary insufficiency, low plasma sodium, or ammonium chloride
toxicity.
- Alkalosis (increased
blood pH) occurs in uncomplicated heart failure itself, in
hyperventilation, in alveolar-capillary block due to associated pulmonary
fibrosis, after mercurial diuresis that causes hypochloremic alkalosis,
or because of potassium depletion.
- Alkalosis (with normal
or increased blood pH) showing increased plasma bicarbonate and
moderately increased pCO after acute correction
of respiratory acidosis is due to CO retention when there is
chloride deficit and usually decreased potassium.
Hypertension
- (Present
in 18% of adults in the United
States)
- Systolic hypertension
- Hyperthyroidism
- Chronic anemia with
hemoglobin <7 gm/dL
- Arteriovenous
fistulas-advanced Paget's disease of bone; pulmonary arteriovenous varix
- Beriberi
- Diastolic hypertension
- Systolic and diastolic
hypertension
- Essential (primary)
hypertension (causes >90% of cases of hypertension).
- Secondary hypertension
(causes <10% of cases of hypertension). Laboratory findings due to the
primary disease. These conditions are often unsuspected and should always
be ruled out, because many of them represent curable causes of
hypertension.
Due To
- Endocrine diseases
- Adrenal
- Pheochromocytoma (<0.64% of cases of
hypertension)
- Aldosteronism (<1% of cases of
hypertension)
- Cushing's syndrome
- Congenital adrenal
hyperplasia (CAH;)
- Pituitary disease
- Signs of hyperadrenal
function
- Acromegaly
- Hyperthyroidism
- Hyperparathyroidism
- Renal diseases
P.117
- Vascular (4% of cases of
hypertension)
- Renal artery stenosis
(usually due to atheromatous plaque in elderly patients and to
fibromuscular hyperplasia in younger patients) (0.18% of cases of
hypertension)
- Nephrosclerosis
- Embolism
- Arteriovenous fistula
- Aneurysm
- Aortitis or coarctation
of aorta with renal ischemia
- Parenchymal
- Glomerulonephritis
- Pyelonephritis
- Polycystic kidneys
- Kimmelstiel-Wilson
syndrome
- Amyloidosis
- Collagen diseases
- Renin-producing renal
tumor (Wilms' tumor; renal hemangiopericytoma)
- Miscellaneous
- Urinary tract
obstructions
- Central nervous system
diseases
- Cerebrovascular accident
- Brain tumors
- Poliomyelitis
- Other
- Toxemia of pregnancy
- Polycythemia
- Acute porphyria
- Drugs, toxins
- Oral contraceptives,
tricyclic antidepressants
- Lead, alcohol
- Licorice ingestion
- In children <18 yrs of
age
|
Renal disease
|
|
|
Cardiovascular disease (e.g.,
coarctation of aorta)
|
|
|
Endocrine (e.g., mineralocorticoid
excess, pheochromocytoma, hyperthyroidism, hypercalcemia)
|
|
|
Miscellaneous (e.g., induced by
traction, after GU tract surgery, associated with sleep apnea)
|
|
|
Essential
|
|
|
- In neonates and young
infants
- Most common
- Renal artery thrombosis
after umbilical artery catheterization
- Coarctation of aorta
- Congenital renal
disease
- Renal artery stenosis
- Less common
- Bronchopulmonary
dysplasia
- Patent ductus
arteriosus
- Intraventricular
hemorrhage
- Laboratory findings
indicating the functional renal status (e.g., urinalysis, BUN, creatinine,
uric acid, serum electrolytes, PSP, creatinine clearance, radioisotope
scan of kidneys, renal biopsy). The higher the uric acid in uncomplicated
essential hypertension, the less the renal blood flow and the higher the
renal vascular resistance.
- Laboratory findings due
to complications of hypertension (e.g., congestive heart failure, uremia,
cerebral hemorrhage, myocardial infarction)
- Laboratory findings due
to administration of some antihypertensive drugs
- Oral diuretics (e.g.,
benzothiadiazines)
- Increased incidence of
hyperuricemia (to 65-75% of hypertensive patients from incidence of
25-35% in untreated hypertensive patients)
- Hypokalemia
- Hyperglycemia or
aggravation of preexisting diabetes mellitus
P.118
- Less commonly, bone
marrow depression, aggravation of renal or hepatic insufficiency by
electrolyte imbalance, cholestatic hepatitis, toxic pancreatitis
- Hydralazine
- Long-term dosage of
>200 mg/day may produce syndrome not distinguishable from SLE.
Usually regresses after drug is discontinued. Antinuclear antibody may
be found in ≤50% of asymptomatic patients.
- Methyldopa
- ≤20% of patients
may have positive results on direct Coombs' test, but relatively few
have hemolytic anemia. When drug is discontinued, Coombs' test may
remain positive for months but anemia usually reverses promptly.
Abnormal liver function tests indicate hepatocellular damage without
jaundice associated with febrile influenza-like syndrome. RA and SLE
tests may occasionally be positive (see Chapter 17).
Rarely, granulocytopenia or thrombocytopenia may occur.
- Monoamine oxidase
inhibitors (e.g., pargyline hydrochloride)
- Wide range of toxic
reactions, most serious of which are
- Blood dyscrasias
- Hepatocellular necrosis
- Diazoxide
- Sodium and fluid retention
- Hyperglycemia (usually
mild and manageable by insulin or oral hypoglycemic agents)
- When hypertension is
associated with decreased serum potassium, rule out
- Primary aldosteronism
- Pseudoaldosteronism (due
to excessive ingestion of licorice)
- Secondary aldosteronism
(e.g., malignant hypertension)
- Hypokalemia due to
diuretic administration
- Potassium loss due to
renal disease
- Cushing's syndrome
Kawasaki Syndrome (Mucocutaneous Lymph Node Syndrome)
- (Variant
of childhood polyarteritis of unknown etiology, with high incidence of
cardiac complications; diagnosis is based on clinical criteria)
- Diagnosis is confirmed by histologic examination of coronary artery (same as in poly-
arteritis nodosa).
- Laboratory changes due to acute myocardial infarction
- Acute phase reactants are
increased (e.g., ESR, CRP, alpha-1-antitrypsin); usually return to normal
after 6-8 wks.
- Leukocytosis
(20,000-30,000/cu mm) with shift to left during first week; lymphocytosis
thereafter; peaks at end of second week; this is a hallmark of the
illness.
- Anemia occurs in ~50% of
patients; reaches nadir about end of second week; improves during
recovery.
- CSF shows increased
mononuclear cells with normal protein and sugar.
- Increased mononuclear
cells in urine; dipstick negative.
- Increased WBC(predominantly PMNs) in joint fluid in patients with
arthritis.
Löffler's
Parietal Fibroplastic Endocarditis
- Eosinophilia ≤70%; may be absent at first but appears sooner or later.
- WBC frequently increased.
- Laboratory findings due
to frequent
- Mural thrombi in heart
and embolization of spleen and lung
- Mitral and tricuspid
regurgitation
Myocardial
Contusion
- (90%
due to motor vehicle accident)
- Increased serum CK-MB (>3%) alone in 15% of cases; combined with ECG
changes in 20% of cases; ECG changes alone in 65% of cases
- Increased serum cardiac troponin I (cTnI) implies some myocardial necrosis and
differentiates increased CK-MB due to skeletal muscle damage. Specificity
= 90% but
P.119
sensitivity = only 30% and positive predictive value =
only 16%. Cardiac troponin T (cTnT) may be increased due to muscle necrosis.
|

|
|
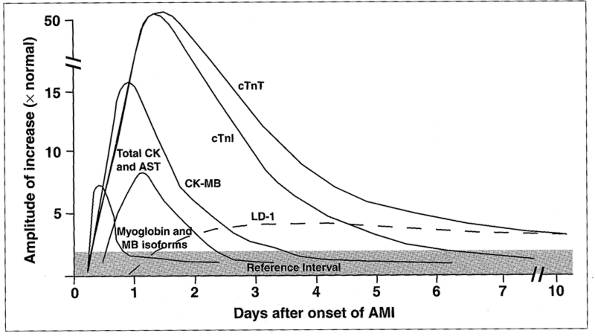
Fig. 5-1. Algorithm for diagnosis of
acute myocardial infarction.
|
Myocardial
Infarction, Acute (AMI)
- See Figs.
5-1 and and Tables 5-1,
and .
- Includes the whole
spectrum of acute coronary syndromes, from silent ischemia, unstable
angina, and "non-Q wave" infarction, to typical AMI.
Diagnostic
Criteria for AMI
- Two of the following
three findings:
- History of ischemic
chest discomfort for ≥30 mins
- Characteristic evolution
of ECG changes
|
|
|
Fig. 5-2. Serial serum cardiac markers
after acute myocardial infarction.
|
- P.120
-
- Typical rise and fall of
cardiac enzymes. Blood should be drawn promptly after onset of symptoms.
Repeat determinations should be made at appropriate intervals (e.g., 4,
8, and 12 hrs) and also if symptoms recur or new signs or symptoms develop.
Changes may indicate extension or additional myocardial infarction (MI)
or other complications (e.g., pulmonary infarction).
Use of
Laboratory Determinations
- For diagnosis when ECG
changes are nondiagnostic (occurs in ~50% of AMI patients) on admission
to emergency room (e.g., masked by bundle branch block or
Wolff-Parkinson-White syndrome) or may not reveal intramural or posterior
or lateral infarcts. False-positive ECG occurs in >10-20% of cases.
- For differential
diagnosis of chest pain.
- To follow the course of
the patient with AMI.
- To estimate prognosis
(e.g., marked elevation of serum enzyme [4-5× normal] correlates with
increased incidence of ventricular arrhythmia, shock, and heart failure,
and with higher mortality).
- For noninvasive
assessment of coronary reperfusion after thrombolytic therapy.
- Utility
of each enzyme depends on time of specimen's collection after onset of
AMI
- Combination of markers
(e.g., serum myoglobin, CK-MB, cTn) and (ratios of) serial changes are
most effective because of uncertainty as to actual duration of myocardial
damage.
Serum
Total Creatine Kinase (CK)
- Use
- Replaced by serum cTn,
CK-MB, myoglobin in various combinations.
- May allow early
diagnosis because increased levels appear 3-6 hrs after onset and
persist≤48 hrs.
- Sensitive indicator
because of large amplitude of change (6-12× normal).
- Interpretation
- Serial total CK has
sensitivity of 98% early in course of MI but false-positive rate of 15%
due to many causes of increased CK.
- Returns to normal by
third day; a poorer prognosis is suggested if the increase lasts more
than 3-4 days. Reinfarction is indicated by an elevated level after the
fifth day after previous return to normal.
P.121
- Useful in differential
diagnosis of chest pain due to diseases often associated with MI or
difficult to distinguish from MI.
|
|
|
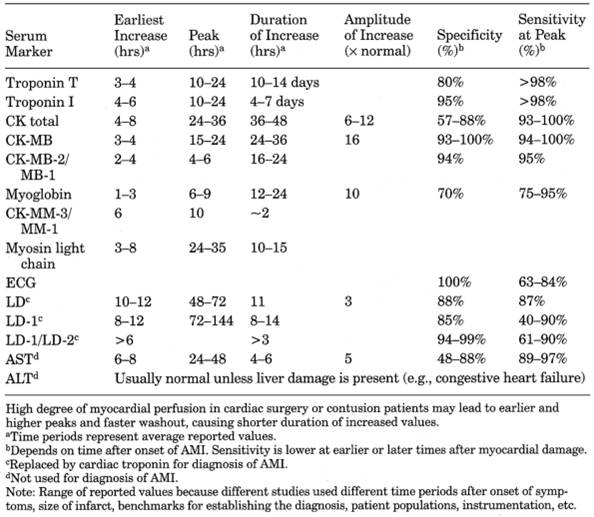
Table 5-1. Summary of Increased Serum
Marker Levels After Acute Myocardial Infarction (AMI)
|
Serial
Serum CK-MB Concentrations
- Use
- Present gold standard
for diagnosis within 24 hrs of onset of symptoms.
- Detect reinfarction or extension of MI after 72 hrs.
- Document reperfusion
after thrombolytic therapy.
- Interpretation
- . In AMI, CK-MB usually is evident at 4-8 hrs, peaks at 15-24 hrs (mean peak
= 16× normal), with sensitivity and specificity each >97% within the
first 48 hrs. By 72 hrs, two-thirds of patients still show some increase
in CK-MB. More frequent sampling (every 6 hrs) is more likely to identify
a peak value. False-negative results may be due to sampling timing (e.g.,
only once in 24 hrs or sampling <4 hrs or >72 hrs after AMI).
- . Diagnosis of AMI is usually confirmed by 8-12 hrs, and sampling beyond 24 hrs is usually
not needed except to detect early reinfarction (especially in patients
receiving thrombolytic therapy).
- . Diagnosis of AMI should not be based on only a single enzyme value.
One criterion for AMI is serial CK-MB measurements 4 hrs apart that show ≥50% increase with at least one sample
greater than upper reference value.
P.122
|
|
|
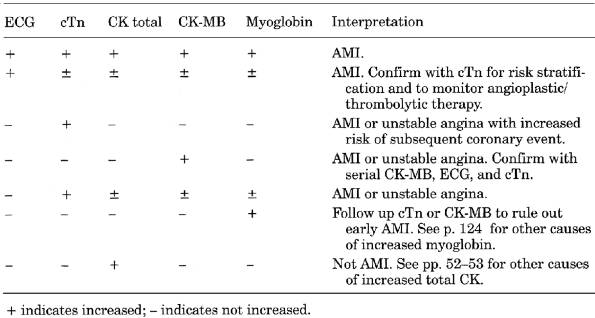
Table 5-2. Interpretation of Markers for
Diagnosis of Acute Myocardial Infarction (AMI)
|
|
|
|
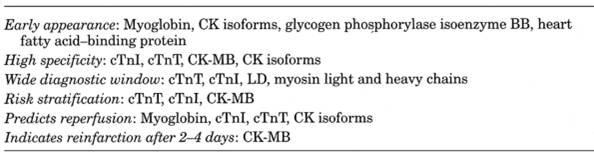
Table 5-3. Characteristics of Serum
Markers for Myocardial Damage
|
- . In ~5% of AMI patients (especially in
older age groups) a peak CK-MB may be the only abnormality, with total CK
and CK-MB still within reference ranges. This is because normal serum
total CK values decline with decreased muscle mass (e.g., with age and
sedentary or bedridden status).
- . Rapid return to
normal makes CK-MB a poor marker >72 hrs after symptoms.
- . Increased CK-MB
with normal total CK may indicate non-Q wave AMI.
- . MB index
(CK-MB/total CK) should be calculated; normal <2.5. For example, with
extreme skeletal muscle injury (e.g., trauma, perioperative condition),
total CK may be >4000 U/L and CK-MB may be ≤40 U/L.
- . CK-MB should be
reported in units as well as percentage, because if injury of both cardiac
and skeletal muscle (e.g., perioperative AMI) is present, CK-MB percentage
may not appear increased.
- . CK-MB mass
immunoassays (preferred method) at 0, 3, and 6 hrs can measure small but
significant serial changes that may still be within the normal range.
CK-MB mass ≥10 µg/L indicates AMI. Serum CK-MB can now be measured
directly in the emergency room with or without total CK, cTn, and
myoglobin.
- . Thrombolytic
therapy should be given within 4-6 hrs of the acute event, at which time
CK-MB may not yet be increased. CK-MB, cTn, and myoglobin measured
initially and at 60 and/or 90 mins after thrombolytic therapy can document
failed reperfusion.
P.123
|
|
60 min
|
|
90 min
|
|
|
Sensitivity
|
Specificity
|
|
Sensitivity
|
Specificity
|
|
CK-MB
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
cTnT
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Myoglobin
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Numbers in parentheses are ratios of
marker values after thrombolytic therapy to pretreatment values.
|
|
CK and
CK-MB May Also Be Increased In
- Diagnostic value of CK-MB
and total CK are diminished after cardiac surgery. A diagnosis of AMI
cannot be made until >12-24 hrs after cardiac surgery; typically AMI
patients have higher peak values of CK, CK-MB, and myoglobin; patients
without AMI have earlier peaks that return to base values more rapidly.
- Increases common after
angioplasty of coronary arteries; may indicate reperfusion.
- Cardiac trauma and
contusions, electrical injury, and inflammatory myocarditis may produce
enzyme changes that cannot be distinguished from those due to AMI. CK-MB
and total CK can be increased with long-term exercise and in chronic
disease.
- No significant increase
after pacemaker implantation or electrical cardioversion.
- If CK-MB is >20% or
persists >48-72 hrs, consider atypical CK-MB.
- Other causes of CK and
CK-MB changes are noted.
- In one protocol the
criteria for AMI are an increasing (above reference range) and then
decreasing CK total and CK-MB in serial specimens drawn on admission and
at 8- or 12-hr intervals; this is considered almost pathognomonic in
patients in whom AMI is strongly suspected; no blood need be collected
after 48 hrs in patients with uneventful course.
- CK-MB in pericardial
fluid may be helpful for postmortem diagnosis of AMI.
Increased
Serum Cardiac Troponins T and I
- Use
- Increased cTn implies
some myocardial necrosis (e.g., anoxia, contusion, inflammation) even
without ECG changes.
- Replace LD testing for
late diagnosis of AMI. May replace CK-MB as gold standard.
- Risk stratification in
patients with chest pain. Sensitive marker for minor myocardial injury in
unstable angina without AMI. Patients with chest pain, normal CK-MB,
nondiagnostic ECG, and detectable cTn have greater risk of later coronary
events.
- Diagnosis of
perioperative AMI when CK-MB may be increased by skeletal muscle injury.
- Serial measurements to
assess reperfusion after thrombolytic therapy. Peak cTn after reperfusion
is related to infarct size.
- Serial values may be
indicator of cardiac allograft rejection.
- Interpretation
- . cTn is about as sensitive as CK-MB during first 48 hrs after AMI;
sensitivity = 33% from 0 to 2 hrs, 50% from 2 to 4 hrs, 75% from 4 to 8
hrs, and approaches 100% from 8 hrs after onset of chest pain. >85%
concordance with CK-MB. Specificity approaches 100%. High sensitivity for
6 days; may remain increased for ~7-10 days.
- . With rapid ELISA
for cTnT, AMI was present in
- 1% of cases with cTnT
<0.1 µg/L
- 28% of cases with cTnT
0.1-0.19 µg/L
- 88% of cases with cTnT
0.2-0.29 µg/L
- 100% of cases with cTnT
>4.0 µg/L3
P.124
- . cTnT may be increased in some patients with skeletal
muscle injury, myotonic dystrophy, and chronic renal failure. cTnI is not increased by skeletal muscle injury, which
makes it more highly specific for myocardial injury; may be detected in
some patients with renal failure.
- . Normal values
exclude myocardial necrosis in patients with increased CK of skeletal
muscle origin (e.g., after arduous physical exercise).
- . Not increased by
uncomplicated coronary angioplasty or electrical cardioversion.
- . Not increased by
pulmonary or orthopedic surgery.
- . Long duration of
increase provides a longer diagnostic window than with CK-MB but may make
it difficult to recognize reinfarction.
- . cTnI increases ~4-6 hrs after AMI and remains
increased for ≤7 days. Rapid (20 mins) test kit using whole blood
is now available.
|
|
Comparative
Sensitivity
|
|
Time after symptom onset in AMI
|
Rapid cTnI
|
CK-MB mass
|
CK-MB activity
|
|
3.5±2.7 hrs
|
|
|
|
|
4 hrs later
|
|
|
|
|
Unstable angina
|
|
|
|
|
Serum
Myoglobin
- Use
- Interpretation
- Increased within 1-3 hrs
in >85% of AMI patients, peaks in ~8-12 hrs (may peak within 1 hr) to
~10× upper reference limit, and becomes normal in ~24-36 hrs or less;
reperfusion causes peak 4-6 hrs earlier.
- May precede release of
CK-MB by 2-5 hrs.
- Sensitivity >95%
within 6 hrs of onset of symptoms.
- Myoglobinuria often occurs.
- Disadvantages
- Two or three blood
samples should be drawn at ~1-hr intervals (myoglobin may be released in
multiple short bursts).
- Wide normal range (6-90
ng/mL).
- Low specificity for AMI
(may also be increased in renal failure, shock, open heart surgery, and
skeletal muscle damage or exhaustive exercise,
or in patients and carriers of progressive muscular dystrophy, but not by
cardioversion, cardiac catheterization, or congestive heart failure).
Values are usually much higher in patients with uremia and muscle trauma
than in those with AMI.
CK
Isoforms
- CK-MB and CK-MM are
sequentially converted in the serum by a carboxypeptidase (CK-MM MM-3 MM-2 MM-1; CK-MB MB-2 MB-1).
- Interpretation
- . CK-MM and CK-MB isoforms parallel CK-MB but rise and peak earlier. MB-2/MB-1 and
MM-3/MM-1 isoform ratios appear to be the most useful, but methodology for
rapid turnaround time is not widely available. Because serum MM-3 is
normally so low, its release from damaged cardiac muscle is readily
evident.
- Diagnostic MM isoform
changes are independent of amount of tissue damage, whereas total CK
activity depends on infarct size.
- MM-3/MM-1 isoform ratio
shows a large change because MM-1 is continually cleared from the blood.
Ratio is ~1.3 in controls but >14 in AMI patients (1.0 is a useful
cutoff value).
- MB-2 >1.0 U/L and
MB-2/MB-1 ratio >1.5 (normal ratio = 1) is specific for AMI within 4-8
hrs of infarct. Ratio is >1.5 within 2-4 hrs in >50% of cases,
within 4-6 hrs in 92%, and by 8 hrs in 100%. MB-2/MB-1 ratio ≤1.0 by
4-6 hrs or normal CK-MB by 10 hrs rules out AMI in 95% of cases.
- MM-3 and MM-3/MM-1 ratio
also increase 2 hrs after intense brief exercise and in marathon runners.
P.125
- CK-MB subforms may also
be increased in severe skeletal muscle damage (e.g., rhabdomyolysis) and
muscular dystrophy.
- Isoform ratios return to
normal by 24 hrs in most patients.
Glycogen
Phosphorylase BB
- Use
- More sensitive early
marker for AMI and unstable angina within 4 hrs after onset of pain than
is CK-MB, cTnT, or myoglobin
- Sensitive marker of
perioperative myocardial injury in coronary artery bypass surgery
Interpretation
- Returns to normal within
24-36 hrs.
- Not widely available.
Additional studies are needed.
- Also being investigated are serum cardiac myosin heavy and light chains, fatty
acid-binding protein, alpha-actin, calcitonin gene-related peptide.
Serum
Lactate Dehydrogenase (LD)
- Use
- Replaced by cTn.
- Prolonged elevation
lasting 10-14 days was formerly used for late diagnosis.
- Interpretation
- Increases in 10-12 hrs,
peaks in 48-72 hrs (~3× normal).
- Increased CK-MB and
LD-1/LD-2 ratio >1 ("flipped" LD) both within 48 hrs (not necessarily
at the same time) is virtually diagnostic of AMI.
- Increased total LD with
flipped LD may also occur in acute renal infarction, hemolysis (e.g.,
hemolytic anemia, pernicious anemia, prosthetic heart valves), some
muscle disorders (e.g., polymyositis, muscular dystrophies, rhabdomyolysis),
pregnancy, some neoplasms (e.g., small cell of lung, prostate, testicular
germ cell); LD >2000 U suggests a poorer prognosis.
Serum
Aspartate Aminotransferase (AST)
- Use
- Replaced by other
enzymes in diagnosis of AMI.
- Interpretation
- AST is increased in
>95% of the patients when blood is drawn at the appropriate time.
- Increase appears within
6-8 hrs, peaks in 24 hrs; level usually returns to normal in 4-6 days.
- Peak level is usually
~200 U (5× normal). Value >300 U and a more prolonged increase suggest
a poorer prognosis.
- Reinfarction is
indicated by a rise that follows a return to normal.
- Serum ALT is usually not
increased unless there is liver damage due to congestive heart failure,
drug therapy, etc.
- Serum ALP (from vascular
endothelium) is increased during reparative phase (4-10 days after onset).
Serum GGT is also increased.
- Leukocytosis is almost
invariable; commonly detected by second day but may occur as early as 2
hrs. WBC is usually 12,000-15,000; ≤20,000 is not rare; sometimes it
is very high. Usually 75-90% PMNs with only a slight shift to the left.
Leukocytosis is likely to develop before fever.
- ESR is increased, usually
by second or third day (may begin within a few hrs); peak rate is in 4-5
days, persists for 2-6 mos. ESR is sometimes more sensitive than WBC, as
increase may occur before fever and persists after temperature and WBC
have returned to normal. Degree of ESR increase does not correlate with
severity or prognosis.
- CRP is usually normal in
unstable angina patients who have a normal cTnT (<0.1 µg/L). Peak CRP
correlates with peak CK-MB.
- Blood lactate is
increased; sensitivity = 55%, specificity = 96% in patients presenting
with acute chest pain.
- Glycosuria and
hyperglycemia occur in ≤50% of patients.
- Glucose tolerance is
decreased.
- Laboratory findings due
to underlying coronary heart disease.
- Laboratory findings due
to sequelae (e.g., congestive heart failure).
P.126
Myocarditis,
Viral
(Routine autopsy
incidence of 1.2-3.5%)
Due To
- Coxsackievirus B (causes
most cases in United States) and coxsackievirus A, echovirus,
poliomyelitis, influenza A and B, cytomegalovirus (CMV), EBV, adenovirus,
rubeola, mumps, rubella, variola, vaccinia, varicella-zoster virus (VZV),
rabies, lymphocytic choriomeningitis, chikungunya, dengue, yellow fever
- Serologic tests for viral antigen, IgM antibody, or changed titer using acute and
convalescent paired sera
- Endomyocardial biopsy of right ventricular muscle showing >5 lymphocytes/HPF
and degeneration of muscle fibers has become major diagnostic tool to
establish diagnosis of myocarditis and rules out other lesions (e.g.,
sarcoidosis).
- Increased serum markers
of myocardial damage is common only in early stages
- cTn sensitivity = 53%,
specificity = 93%
- CK-MB and CK total
<10% sensitivity
- Increased acute phase
reactants (e.g., ESR, CRP, mild to moderate leukocytosis)
Myxoma
of Left Atrium
- Anemia that is hemolytic in type and mechanical in origin (due to local
turbulence of blood) should be sought and may be severe. Bizarre
poikilocytes may be seen in blood smear. Reticulocyte count may be
increased. Other findings may reflect effects of hemolysis or compensatory
erythroid hyperplasia. The anemia is recognized in ~50% of patients with
this tumor. Increased serum LD reflects hemolysis.
- Serum gamma globulin is
increased in ~50% of patients. IgG may be increased.
- Increased ESR is a
reflection of abnormal serum proteins.
- Platelet count may be
decreased (possibly the cause here also is mechanical) with resultant
findings due to thrombocytopenia.
- Negative blood cultures
differentiate this tumor from bacterial endocarditis.
- Occasionally WBC is increased,
and CRP may be positive.
- Laboratory findings due
to complications
- Emboli to various organs
(increased AST may reflect many small emboli to striated muscle)
- Congestive heart failure
- These findings are
reported much less frequently in myxoma of the right atrium, which is more
likely to be accompanied by secondary polycythemia than by anemia.
Pericardial
Effusion, Chronic
- See Table
6-2 on body fluids.
- Laboratory findings due
to underlying disease (e.g., TB, myxedema, metastatic tumor, uremia, SLE).
Rarely due to severe anemia, scleroderma, polyarteritis nodosa, Wegener's
granulomatosis, RA, irradiation therapy, mycotic or
viral infections, primary tumor of heart, African endomyocardial fibrosis,
idiopathic causes.
Pericarditis,
Acute
Laboratory
Findings Due to Primary Disease
- Active rheumatic fever
(40% of patients)
- Bacterial infection (20%
of patients)
- Other infections (e.g.,
viral [especially coxsackievirus B], rickettsial, parasitic,
mycobacterial, fungal)
- Viruses are most common
infectious causes.
- Uremia (11% of patients)
- Benign nonspecific
pericarditis (10% of patients)
- Neoplasms (3.5% of
patients)
- Collagen disease (e.g.,
SLE, polyarteritis nodosa) (2% of patients)
- Acute myocardial
infarction, postcardiac injury syndrome
P.127
- Trauma
- Myxedema
- Others (e.g.,
hypersensitivity, unknown origin or in association with various syndromes)
- WBC is usually increased
in proportion to fever; normal or low in viral disease and tuberculous
pericarditis; markedly increased in suppurative bacterial pericarditis
- Examination of aspirated
pericardial fluid (see Table 6-1)
Phlebothrombosis
- Tests indicate recent
extensive clotting of any origin (e.g., postoperative status).
- D-dimer test (see Pulmonary Embolism and Infarction).
- Staphylococcal clumping
test measures breakdown products of fibrin in serum; these indicate the
presence of a clot that has begun to dissolve. Sensitivity = 88%,
specificity = 66% using venography as gold standard.
- Serial dilution
protamine sulfate test measures the presence of a fibrin monomer that is
one of the polymerization products of fibrinogen. It is less sensitive
than the staphylococcal clumping test but indicates clotting earlier.
- Laboratory findings of pulmonary infarction should be sought as evidence of
embolization.
Polyarteritis
Nodosa
- Tissue biopsy is basis for diagnosis
- Findings on biopsy of
small or medium-sized artery.
- Findings in random skin
and muscle biopsy are confirmatory in 25% of patients; most useful when
taken from area of tenderness; if no symptoms are present, pectoralis major
is the most useful site.
- Testicular biopsy is
useful when local symptoms are present.
- Lymph node and liver
biopsies are usually not helpful.
- Renal biopsy is not
specific; often shows glomerular disease.
- Increased BUN or
creatinine; uremia occurs in 15% of patients.
- Hepatitis B surface
antigen (HBsAg) is present in 20-40% of adult patients.
- p-ANCA is positive in 70% of
patients; rarely reflects disease activity.
- Increased WBC
(≤40,000/cu mm) and PMNs. A rise in eosinophils takes place in 25%
of patients and is sometimes very marked; it usually occurs in patients
with pulmonary manifestations.
- ESR and CRP are
increased.
- Mild anemia is frequent;
it may be hemolytic anemia with positive Coombs' test.
- Urine is frequently
abnormal.
- Albuminuria (60% of
patients)
- Hematuria (40% of
patients)
- "Telescoping" of
sediment (variety of cellular and noncellular casts)
- Serum globulins are
increased.
- Abnormal serum proteins
occasionally occur. Biological false-positive test for syphilis,
circulating anticoagulants, cryoglobulins, macroglobulins, etc., occurs.
- Laboratory findings due
to organ involvement by arteritis may be present (e.g., GU, pulmonary, GI,
neurologic in >75% of patients).
Prosthetic
Heart Valves
- Complications
- Hemolysis-increased
serum LD, decreased haptoglobin, reticulocytosis are usual. Severe
hemolytic anemia is uncommon and suggests leakage due to partial
dehiscence of valve or infection.
- Prosthetic valve
infection
- Early (<60 days
after valve replacement)-usually due to Staphylococcus
epidermidis, S. aureus, gram-negative
bacteria, diphtheroids, fungi; occasionally due to Mycobacteria
and Legionella. 30-80% mortality.
- Late (>60 days
postoperatively)-usually due to streptococci. S.
epidermidis is common up to 12 mos after surgery. 20-40%
mortality.
- . Blood culture positive in >90% of patients unless received antibiotic
therapy, infection involves fastidious organism (e.g., HACEK [Haemophilus-Actinobacillus-Cardiobacterium-Eikenella-Kingella]),
P.128
or identification requires special technique (e.g., Rickettsia, fungi, mycobacteria, Legionella).
- Surgery is indicated if
blood culture is positive after 5 days of appropriate antimicrobial
therapy or infection is recurrent. Infection with
organisms other than Streptococcus usually
require valve replacement.
- Complications of
anticoagulant therapy
Rheumatic
Fever, Acute5
- Increased serum cTn implies some myocardial necrosis due to myocarditis.
- Laboratory confirmation of preceding group A streptococcal infection
- Increased titer of
antistreptococcal antibodies
- Positive throat culture
for group A Streptococcus and recent scarlet
fever
- Serologic tests-see
below
- Serologic titers: one of the following is elevated in 95% of patients with acute
rheumatic fever; if all are normal, a diagnosis of rheumatic fever is less
likely.
- ASOT increase indicates
recent group A Streptococcus
pharyngitis within the last 2 mos. Increased titer develops only after
the second week and reaches a peak in 4-6 wks. Increasing titer is more
significant than a single determination. Titer is usually >250 U; more
significant if >400-500 U. A normal titer helps to rule out clinically
doubtful rheumatic fever. Sometimes ASOT is not increased even when other
titers are increased. Height of titer is not related to severity; rate of
fall is not related to course of disease.
- Anti-DNase B assay
should also be performed because >15% of patients with acute rheumatic
fever do not have an increased ASOT. This assay is superior to ASOT in
detecting antibodies after group A streptococcal skin infections and is
less prone to false-positive reactions; longer period of reactivity is
helpful in patients with isolated chorea or carditis, who may have a long
latent period before manifesting rheumatic fever during which ASOT may
have returned to normal.
- Antihyaluronidase titer
of 1000-1500 U follows recent group A
streptococcal disease and ≤4000 U with rheumatic fever. Average
titer is higher in early rheumatic fever than in subsiding or inactive
rheumatic fever or nonrheumatic streptococcal disease or nonstreptococcal
infections. Antihyaluronidase titer is increased as often as ASOT and
antifibrinolysin titer.
- Antifibrinolysin
(antistreptokinase) titer is increased in rheumatic fever and in recent
hemolytic streptococcus infections.
- Acute phase reactants (ESR, CRP, increased WBC) are
minor manifestations.
- ESR increase is a sensitive
test of rheumatic activity; ESR returns to normal after adequate
treatment with ACTH or salicylates. It may remain increased after WBC
becomes normal. It is said to become normal with onset of congestive
heart failure even in the presence of rheumatic activity. It is normal in
uncomplicated chorea alone.
- CRP parallels ESR.
- WBC may be normal but
usually is increased (10,000-16,000/cu mm) with shift to the left;
increase may persist for weeks after fever subsides. Count may decrease
with salicylate and ACTH therapy.
- Serum proteins are
altered, with decreased serum albumin and increased alpha
and gamma globulins. (Streptococcus group A infections do not increase alpha
globulin.) Fibrinogen is increased.
- Anemia (Hb usually 8-12
gm/dL) is common; gradually improves as activity subsides; microcytic
type. Anemia may be related to increased plasma volume that occurs in
early phase of acute rheumatic fever.
- Urine: A slight febrile
albuminuria is present. Often mild abnormality of protein, casts, RBCs,
WBCs indicates mild focal nephritis. Concomitant GN appears in ≤2.5%
of cases.
P.129
- Blood cultures are
usually negative. Occasional positive culture is found in 5% of patients
(bacteria usually grow only in fluid media, not on solid media), in
contrast to bacterial endocarditis.
- Throat culture is often
negative for group A streptococci.
- Serum AST may be
increased, but ALT is normal unless the patient has cardiac failure with
liver damage.
- Determine clinical
activity-follow ESR, CRP, and WBC. Return to normal should be seen in 6-12
wks in 80-90% of patients; it may take ≤6 mos. Normal
findings do not prove inactivity if patient is receiving hormone therapy.
When therapy is stopped after findings have been suppressed for 6-8 wks, a
mild rebound may be seen for 2-3 days followed by a return to normal.
Relapse after cessation of therapy occurs within 1-8 wks.
Shock
- Leukocytosis is common,
especially with hemorrhage. Leukopenia may be present when shock is
severe, as in gram-negative bacteremia. Circulating eosinophils are
decreased.
- Hemoconcentration (e.g.,
dehydration, burns) or hemodilution (e.g., hemorrhage, crush injuries, and
skeletal trauma) takes place.
- Acidosis appears when
shock is well developed, with increased blood lactate, low serum sodium,
low CO -combining power with
decreased alkaline reserve.
- Blood pH is usually
relatively normal but may be decreased. BUN and creatinine may be
increased.
- Serum potassium may be
increased.
- Hyperglycemia occurs
early.
- Urine examination
- Volume: Normovolemic
patients have output ≥50 mL/hr; cause should be investigated if
<25-30 mL/hr. In hypovolemia, normal kidney may lower 24-hr urine
output to 300-400 mL.
- Specific gravity:
>1.020 with low urine output suggests patient is fluid depleted.
<1.010 with low urine output suggests renal insufficiency. Specific
gravity depends on weight rather than concentration of solutes; therefore
it is more affected than osmolarity by high-molecular-weight substances
such as urea, albumin, and glucose.
- Osmolarity: Hypovolemia
is suggested by high urine osmolarity and urine-plasma osmolarity ratio
of ≥1:2. Renal failure is suggested by low urine osmolarity with
oliguria and urine/plasma osmolarity ratio of ≤1:1.
Systemic
Capillary Leak Syndrome6
- (Very
rare recurring idiopathic disorder in adults with sudden transient
extravasation of <70% of plasma; very high morbidity and mortality;
hypotension is part of triad)
- Hemoconcentration (e.g.,
leukocytosis; Hb may be ~25 gm/dL)
- Hypoalbuminemia
- Monoclonal gammopathy
(especially IgG with kappa or lambda light chain) without evidence of
multiple myeloma is often present. Some patients may progress to multiple
myeloma.
- Laboratory findings due
to complications (e.g., rhabdomyolysis, acute tubular necrosis,
pleural/pericardial effusion)
Takayasu's
Syndrome (Arteritis)
- Increased ESR in ~75% of
cases during active disease but normal in only one-half during remission
- WBC usually normal
- Serum proteins abnormal
with increased gamma globulins (mostly composed of IgM)
- Female patients have a
continuous high level of urinary total estrogens (rather than the usual
rise during luteal phase after a low excretion during follicular phase).
- Laboratory tests not
useful for diagnosis or to guide management.
- Diagnosis is established by characteristic arteriographic changes or histologic
examination.
P.130
Thromboangiitis
Obliterans (Buerger's Disease)
- (Vascular
inflammation and occlusion of intermediate-sized arteries and veins of
extremities)
- Laboratory tests are
usually normal.
Thrombophlebitis,
Septic
- Laboratory findings due
to associated septicemia
- Increased WBC (often
>20,000/cu mm) with marked shift to left and toxic changes in
neutrophils.
- DIC may be present.
- Respiratory alkalosis
due to ventilation-perfusion abnormalities with hypoxia. Significant
acidosis indicates shock.
- Azotemia.
- Positive blood culture (S. aureus is most frequent organism; others are Klebsiella, Pseudomonas aeruginosa, enterococci, Candida).
- Laboratory findings due
to complications (e.g., septic pulmonary infarction)
- Laboratory findings due
to underlying disease
Transplant
Rejection (Acute) of Heart
- Endocardial biopsy to determine acute
rejection and follow effects of therapy has no substitute.
- Increasing ESR and WBC
- Increased isoenzyme LD-1
as amount (>100 IU) and percentage (35%) of total LD during first 4 wks
after surgery
- These findings are
reversed with effective immunosuppressive therapy. Total LD continues to
be increased even when LD-1 becomes normal.
- Chronic rejection is accelerated
coronary artery atherosclerosis.
Valvular
Heart Disease
- Laboratory findings due
to associated or underlying or predisposing disease (e.g., syphilis,
rheumatic fever, carcinoid syndrome, genetic disease of mucopolysaccharide
metabolism, congenital defects)
- Laboratory findings due
to complications (e.g., heart failure, bacterial endocarditis, embolic
phenomena)
Vasculitis,
Classification
By
Etiology
- Primary
- Polyarteritis nodosa
- Wegener's granulomatosis
- Giant cell arteritis
- Hypersensitivity vasculitis
- Secondary
- Infections
- Bacteria (e.g.,
septicemia due to Gonococcus or Staphylococcus)
- Mycobacteria
- Viruses (e.g., CMV,
HBV)
- Rickettsia (e.g., Rocky Mountain
spotted fever)
- Spirochetes (e.g.,
syphilis, Lyme disease)
- Associated with
malignancy (e.g., multiple myeloma, lymphomas)
- Connective tissue
diseases
- RA
- SLE
- Sjögren's syndrome
- Diseases that may
simulate vasculitis (e.g., ergotamine toxicity, cholesterol embolization,
atrial myxoma)
P.131
By
Size of Involved Vessel (Noninfectious Vasculitis)
- Large vessel
- Takayasu's arteritis
- Giant cell (temporal)
arteritis
- Medium-sized vessel
- Polyarteritis nodosa
- Kawasaki's disease
- Primary granulomatous
CNS vasculitis
- Small vessel
- ANCA-associated
vasculitis
- Wegener's
granulomatosis
- Churg-Strauss syndrome
- Drug induced
- Microscopic
polyangiitis
- Immune complex-type
vasculitis
- Henoch-Schönlein
purpura
- Cryoglobulinemia
- Rheumatoid vasculitis
- SLE
- Sjögren's syndrome
- Goodpasture's syndrome
- Behēet's disease
- Drug induced
- Serum sickness
- Paraneoplastic vasculitis (lymphoproliferative, myeloproliferative,
carcinoma)
- Inflammatory bowel
disease
Wegener's
Granulomatosis7
- (Necrotizing
granulomatous vasculitis affecting respiratory tract; disseminated form
shows renal involvement)
- Diagnosis is established by biopsy of affected tissue with cultures and special
stains that exclude mycobacterial and fungal infection.
Antineutrophil
Cytoplasmic Antibodies (ANCA)
- Use
- Aid in diagnosis and
classification of various vasculitis-associated and autoimmune disorders.
- Interpretation
- c-ANCA (anti-proteinase 3; coarse diffuse cytoplasmic
pattern) is highly specific (>90%) for active Wegener's granulomatosis.
Sensitivity >90% in systemic vasculitic phase ~65% in predominantly
granulomatous disease of respiratory tract, ~30% during complete
remission. Height of ELISA titer does not correlate with disease activity;
high titer may persist during remission for years. Also occasionally found
in other vasculitides (polyarteritis nodosa, microscopic polyangiitis
[e.g., lung, idiopathic crescentic and pauci-immune GN], Churg-Strauss
vasculitis).
- p-ANCA (against various proteins [e.g.,
myeloperoxidase, elastase, lysozyme], perinuclear pattern) occurs only
with fixation in alcohol, not formalin. Positive result should be
confirmed by ELISA. Has poor specificity and 20-60% sensitivity in a
variety of autoimmune diseases (microscopic polyangiitis, Churg-Strauss
vasculitis, SLE, inflammatory bowel disease, Goodpasture's syndrome,
Sjögren's syndrome, idiopathic GN, chronic infection). However, pulmonary
small vessel vasculitis is strongly linked with myeloperoxidase antibodies.
- Both p-ANCA and c-ANCA
may be found in non-immune mediated polyarteritis and other vasculitides.
- Atypical pattern (neither c-ANCA or p-ANCA; unknown target antigens) has
poor specificity and unknown sensitivity in various conditions (e.g., HIV
infection, endocarditis, cystic fibrosis, Felty's syndrome, Kawasaki syndrome,
ulcerative colitis, Crohn's disease).
P.132
- Laboratory findings
reflecting specific organ involvement
- Kidneys-renal disease in
~80% of cases. Hematuria (>5 RBCs/HPF),
proteinuria, azotemia. Nephrosis or chronic nephritis may occur. Most
patients develop renal insufficiency. Biopsy most frequently shows focal necrotizing GN with crescent formation; coarse
granular pattern with immunofluorescent staining. Biopsy is important to
define extent of disease.
- CNS.
- Respiratory tract.
- Heart.
- Nonspecific laboratory
findings
- Normochromic anemia,
thrombocytosis, and mild leukocytosis occur in 30-40% of patients;
eosinophilia may occur but is not a feature. Leukopenia or thrombocytopenia occur only during cytotoxic therapy.
- ESR is increased in 90%
of cases, often to very high levels; CRP level correlates with disease
activity even better than ESR.
- Serum globulins (IgG and
IgA) are increased in up to 50% of cases.
- Serum C3 and C4
complement levels may be increased.
- RF may be present in low
titer in two-thirds of cases.
- ANA is negative.
- Laboratory findings due
to secondary infection (usually staphylococcal) of sinus, mucosal,
pulmonary lesions.
- Laboratory findings due
to therapy (e.g., bladder cancer and sterility due to cyclophosphamide
therapy).
REFERENCES
1. Included in American College of Rheumatology 1990 criteria
for classification of vasculitis. Arthritis Rheum .
2. Stewart JT, et al. Early noninvasive identification of failed reperfusion after
intravenous thrombolytic therapy in acute myocardial infarction. J Am Coll Cardiol .
3. Gerhardt W, et al. An
improved rapid troponin T test with a decreased detection limit: a multicentre
study of the analytical and clinical performance in suspected myocardial
damage. Scand J Clin Lab Invest .
4. Heeschen C, et al.
Analytical performance and clinical application of new rapid bedside assay for
the detection of serum cardiac troponin I. Clin Chem .
5. Special Writing Group,
Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on
Cardiovascular Disease in the Young, American Heart Association. Guidelines for
the diagnosis of rheumatic fever: Jones Criteria, 1992 update. JAMA .
6. Tahirkheli NK, Greipp
PR. Treatment of the systemic capillary leak syndrome with terbutaline and
theophylline. Ann Intern Med .
7. Included in American College of Rheumatology 1990 criteria
for classification of vasculitis. Arthritis Rheum .