Endocrine Diseases
General
Principles In Diagnosis of Endocrine Diseases
- Perform stimulatory tests
if hypofunction is suspected and suppression tests if hyperfunction is
suspected.
- Suppression tests
suppress normal glands but not autonomous secretion (e.g., functioning
neoplasm).
- Obtaining multiple or
pooled samples of baseline specimens and drawing specimens from indwelling
lines are often required to obtain optimal specimens.
- Patient preparation is
particularly important for hormone studies, the results of which may be
markedly affected by many factors such as stress, position, fasting state,
time of day, preceding diet, and drug therapy; all of these should be
recorded on the laboratory test requisition form and discussed with the
laboratory before test ordering.
- Appropriate (e.g.,
frozen) and timely transportation to laboratory and preparation of
specimen (e.g., separation of serum may be vital for some tests) are
important.
- No single test adequately
reflects the endocrine status in all conditions.
Tests
of Thyroid Function
- Thyroid function tests
are not indicated for screening programs without
suspicion of thyroid disease (overall yield ~0.5%; varies from 0% in young
men to 1% in women aged >40 yrs). Indicated in certain populations such
as newborns (mandatory), those with strong family history of thyroid
disease, elderly, women 4–8 wks postpartum, patients with autoimmune
diseases (e.g., Addison's disease, type I diabetes mellitus). May be
useful in some women aged >40 yrs with nonspecific complaints.
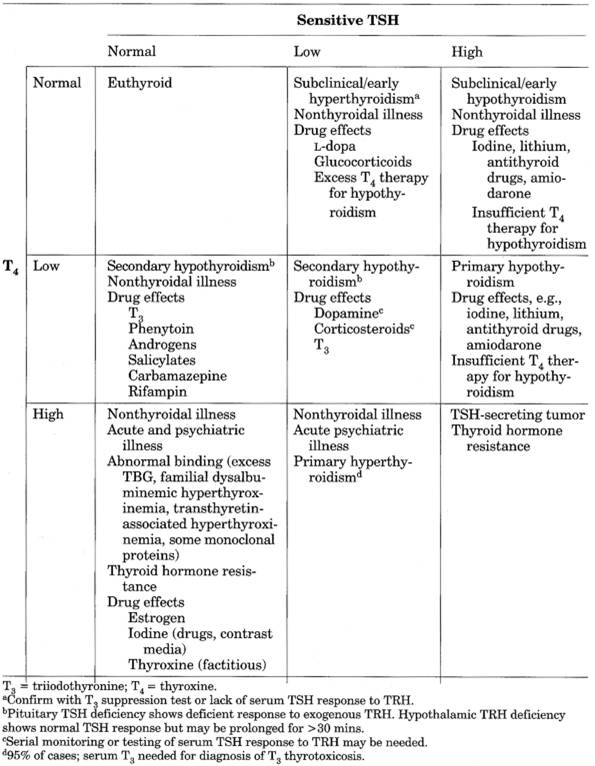
- Sensitive TSH complemented
by free thyroxine index (FTI) are recommended tests for diagnosis and
follow-up of most patients with thyroid disorders (Table
13-1).
Calcitonin
Use
- Basal fasting level may
be increased in patients with medullary carcinoma of the thyroid even when
no mass is palpable in the thyroid. Circadian rhythm with rise to peak
after lunchtime. Basal level is normal in approximately one-third of
medullary carcinoma cases.
- Basal calcitonin levels
- Levels >2000 pg/mL
are almost always associated with medullary carcinoma of thyroid, with
rare cases due to obvious renal failure or ectopic production of
calcitonin.
- Levels of 500–2000 pg/mL
generally indicate medullary carcinoma, renal failure, or ectopic
production of calcitonin.
- Levels of 100–500 pg/mL
should be interpreted cautiously with repeat assays and provocative
tests; if these and repeat tests in 1–2 mos are still abnormal, some
authors recommend total thyroidectomy.
- Normal basal levels:
Males ≤19 pg/mL; females ≤14 pg/mL.
- Calcium infusion and/or
pentagastrin injection are used as provocative tests in patients with
normal basal levels for whom the index of suspicion is high, e.g., those
with a
P.570
family history of thyroid carcinoma, a calcified thyroid mass,
pheochromocytoma, hyperparathyroidism, hypercalcemia, amyloid-containing
metastatic carcinoma of unknown origin, or facial characteristics of the
mucosal neuroma syndrome. Normally level should not rise above 0.2 ng/mL.
Pentagastrin stimulation is more 18118f515s sensitive than calcium stimulation.
|

|
|
Table 13-1. Sensitivity and Specificity
of Thyroid Function Tests
|
- To detect recurrence of
medullary carcinoma or metastases after the primary tumor has been removed
or to confirm complete removal of the tumor if basal calcitonin has been
previously increased.
Increased
in Some Patients with
- Carcinoma of lung,
breast, islet cell, or ovary, and carcinoid due to ectopic production
- Hypercalcemia of any
cause stimulating calcitonin production
- Z-E syndrome
- PA
- Acute or chronic
thyroiditis
- Chronic renal failure
Perchlorate
Washout Test
- Perchlorate is given 2–4
hrs after administration of I and RAIU is calculated
before and at intervals after perchlorate administration.
Use
- Decreased uptake >10%
from peak value is positive test indicating an organification defect as
the cause of hypothyroidism. Free iodide is present within the thyroid in
such patients. Perchlorate blocks the trapping mechanism, causing rapid
discharge of iodine so that RAIU within the thyroid diminishes. Normal
thyroid gland contains very little inorganic iodine.
Reverse
Triiodothyronine (Rt
(Hormonally inactive isomer of T
Use
- Largely replaced by newer
tests
- Usually increased in
hyperthyroidism and increased serum TBG; often decreased in hypothyroidism
but overlaps with normal range.
- Has been suggested to
distinguish “sick thyroid” patients who are euthyroid (usually normal in
euthyroid patients) from true hypothyroid cases, but serum TSH may be more
reliable.
P.571
|
|
|
Table 13-2. Free Thyroxine (T ) and Thyroid-Stimulating Hormone (TSH)
Levels in Various Conditions
|
Thyroid-Stimulating
Hormone Sensitive (Thyrotropin; Tsh)
- (Hormone
secreted by anterior pituitary; third- and fourth-generation assay
detection limits are 0.01 mU/L and 0.001 mU/L, respectively)
- See Table
13-2, and Fig. 13-1.
- Euthyroid: 0.3–5.0 mU/L
P.572
- Possible hypothyroid:
>5.0 mU/L
- Possible hyperthyroid:
<0.10 mU/L
- Borderline: 0.10–0.29
mU/L
Use
- Screening for
euthyroidism—normal level in stable ambulatory patient not on interfering
drugs excludes thyroid hormone excess or deficiency. Has been recommended
as the initial test of thyroid function rather than T
- Screening is not
recommended for asymptomatic persons without suspicion of thyroid disease
or for hospital patients with acute medical or psychiatric illness.
- Initial screening and
diagnosis for hyperthyroidism (decreased to undetectable levels except in
rare TSH-secreting pituitary adenoma) and hypothyroidism
|

|
|
Table 13-3. Thyroid Function Tests in
Various Conditions
|
|

|
|
Table 13-3. (continued)
|
- Second-generation or rate
assay is required to determine TSH <0.10 mU/L.
- Especially useful in
early or subclinical hypothyroidism before the patient develops clinical
findings, goiter, or abnormalities of other thyroid tests
- Differentiation of
primary (increased levels) from central (pituitary or hypothalamic)
hypothyroidism (decreased levels)
- Monitor adequate thyroid
hormone replacement therapy in primary hypothyroidism, although T
may be mildly increased; up to 6–8 wks before TSH becomes normal. Serum
TSH suppressed to normal level is the best monitor of dosage of thyroid
hormone for treatment of hypothyroidism.
- Monitor adequate thyroid
hormone therapy to suppress thyroid carcinoma (should suppress to <0.1
mU/L) or goiter or nodules (should suppress to subnormal levels). Third-
or fourth-generation assays are required to allow closer titration to
balance inhibition of functioning tumor against induced hyperthyroidism.
- Help differentiate
euthyroid sick syndrome from primary hypothyroid patients. Sensitive TSH
is only very slightly depressed in euthyroid sick patients but usually
significantly depressed in true thyroid disorder.
- Replace TRH stimulation
test in hyperthyroidism because most patients with euthyroid TSH level
have a normal TSH response and patients with undetectable TSH level almost
never respond to TRH stimulation
- In very early cases with
only marginal elevation, the TRH stimulation test may be preferred.
May
Not Be Useful
- As a
single test to evaluate thyroid status of hospitalized or severely ill
patients
- To monitor efficacy of
thyroid ablation therapy for hyperthyroidism because TSH remains
suppressed until T declines significantly;
T or free T is test of choice.
Interferences
- Dopamine or high doses of
glucocorticoids may cause false-normal values in primary hypothyroidism
and may suppress TSH in nonthyroid illness.
- Presence of RF, human
antimouse antibodies, and thyroid hormone autoantibodies may produce
spurious results, especially in patients with autoimmune disorders
(≤10%).
P.574
|

|
|
Fig. 13-1. Algorithm for thyroid function
testing. (D = decreased; I = increased; N = normal.)
|
P.575
Increased
In
- Primary untreated
hypothyroidism. Increase is proportionate to the degree of hypofunction,
varying from 3× normal in mild cases to 100× normal in severe myxedema. A
single determination is usually sufficient to establish the diagnosis.
- Patients with
hypothyroidism receiving insufficient thyroid hormone replacement therapy
- Patients with Hashimoto's
thyroiditis, including those with clinical hypothyroidism and about
one-third of those patients who are clinically euthyroid
- Use of various drugs
(e.g., amphetamine abuse)
- Iodine containing drugs
(e.g., iopanoic acid, ipodate, amiodarone)
- Dopamine antagonists
(e.g., metoclopramide, domperidone, chlorpromazine, haloperidol)
- Other conditions (test is
not clinically useful)
- Iodide-deficiency goiter
- Iodide-induced goiter or
lithium treatment
- External neck
irradiation
- Post–subtotal
thyroidectomy
- Neonatal period
- Thyrotoxicosis due to
pituitary thyrotroph adenoma or pituitary resistance to thyroid hormone
- Euthyroid sick syndrome,
recovery phase
- TSH antibodies
- Increased in first 2–3
days of life due to postnatal TSH surge
Decreased
In
- Hyperthyroidism due to
- Toxic multinodular
goiter
- Autonomously functioning
thyroid adenoma
- Ophthalmopathy of
euthyroid Graves' disease
- Treated Graves' disease
- Thyroiditis
- Extrathyroidal thyroid
hormone source
- Factitious
- Overreplacement of
thyroid hormone in treatment of hypothyroidism
- Secondary pituitary or
hypothalamic hypothyroidism
- Euthyroid sick patients
- Acute psychiatric illness
- Severe dehydration
- Drug effect, especially
large doses—use free T for evaluation
- Glucocorticoids,
dopamine, dopamine agonists (bromocriptine), levodopa, T replacement therapy, apomorphine, pyridoxine; T may be normal or low.
- Antithyroid drug for
thyrotoxicosis, especially early in treatment; T may be normal or low.
- Assay interference,
e.g., antibodies to mouse IgG, autoimmune disease.
- First trimester of
pregnancy
May Be
Normal In
- Central hypothyroidism
- Recent rapid correction
of hyperthyroidism or hypothyroidism
- Pregnancy
- Phenytoin therapy
- In
absence of hypothalamic or pituitary disease, normal TSH excludes primary
hypothyroidism
Thyroglobulin
(Tg)
- (Cannot
compare thyroglobulin values using different assays or assays from
different laboratories)
- See Table
13-3.
P.576
Use
- To assess the presence
and possibly the extent of residual, recurrent, or metastatic follicular
or papillary thyroid carcinoma after therapy. In patients with these
carcinomas treated with total thyroidectomy or radioactive iodine and
taking thyroid hormone therapy, Tg is undetectable if functional tumor is
absent but detected by sensitive immunoassay if functional tumor is
present. Tg correlates with tumor mass, with highest values in patients
with metastases to bones and lungs.
- Diagnosis of factitious
hyperthyroidism. Tg is very low or not detectable in factitious
hyperthyroidism and high in all other types of hyperthyroidism (e.g.,
thyroiditis).
- Not recommended for
initial diagnosis of thyroid carcinomas.
- Do not use in patients
with preexisting thyroid disorders.
- Predict outcome of
therapy for hyperthyroidism; higher remission rates in patients with lower
Tg values. Failure to become normal after drug-induced remission suggests
relapse after drugs are discontinued.
- Diagnosis of thyroid
agenesis in newborn
- Presence in pleural
effusions indicates metastatic differentiated thyroid cancer.
Interferences
- Thyroglobulin
autoantibodies interferes with the test; patients' serum must always first
be screened for these antibodies.
Increased
In
- Most patients with
differentiated thyroid carcinoma but not those with undifferentiated or
medullary thyroid carcinomas
- Patients with
hyperthyroidism; rapid decline after surgical treatment. Gradual decline
after radioactive iodine treatment.
- Patients with subacute
thyroiditis
- Some patients with
nontoxic nodular goiter
- Patients with marked
liver insufficiency
Decreased
In
- Thyroid agenesis in
newborn
Thyroid
Autoantibody Tests
(Antimicrosomal
[also called thyroid peroxidase] and antithyroglobulin autoantibodies)
Use
- Positive in almost all
cases of Hashimoto's disease and ~80% of Graves' disease. Very high titer
is pathognomonic of Hashimoto's thyroiditis but absence does not exclude
Hashimoto's thyroiditis. Titer>1 to 1000 occurs virtually only in
Graves' disease or Hashimoto's thyroiditis. Significant titer of microsome
antibodies indicates Hashimoto's thyroiditis or postpartum thyroid
dysfunction.
- To distinguish subacute
thyroiditis from Hashimoto's thyroiditis, as antibodies are more common in
the latter
- Hashimoto's thyroiditis
is very unlikely cause of hypothyroidism in the absence of microsomal and
Tg antibodies.
- Significant titer of
microsomal and Tg antibodies in euthyroid patient with unilateral
exophthalmos suggests the diagnosis of euthyroid Graves' disease.
- Occasionally useful to
distinguish Graves' disease from toxic multinodular goiter when physical
findings are not diagnostic.
- Graves' disease with
elevated titers of antimicrosomal antibodies should direct surgeon to
perform a more limited thyroidectomy to avoid late postthyroidectomy
hypothyroidism.
- Results of Tg antibody
test are less frequently positive than those of microsomal antibody test
in autoimmune thyroid disease.
- Tg antibodies may
interfere with assay for serum Tg.
P.577
- Thyroid receptor antibody
test mainly used in Graves' disease, especially as a predictor of relapse
of hyperthyroidism.
Increased
In
- Occasionally positive in
papillary-follicular carcinoma of thyroid, subacute thyroiditis (briefly),
lymphocytic (painless) thyroiditis (in ~60% of patients).
- Primary thyroid lymphoma
often yields very high titers; should suggest need for biopsy in elderly
patient with a firm, enlarging thyroid.
- Positive in 7% of normal
population, reaching peak of 15% in females in sixth decade
- Other autoimmune diseases
(e.g., PA, RA, SLE, myasthenia gravis)
Thyroid
Uptake of Radioactive Iodine (Raiu)
- See Table
13-3.
- A tracer dose of I or I is administered orally,
and the radioactivity over the thyroid is measured at specific time
intervals (e.g., 2–6 hrs and again at 24 hrs). The percentage of
administered iodine in the thyroid is an index of thyroid trapping and
organification of iodide.
- Normal uptake is 9–19% in
1 hr; 7–25% in 6 hrs; 5–30% in 24 hrs. Varies with local iodine intake.
40–70% of administered dose is excreted in urine in 24 hrs. Technetium 99
( Tc) is a measure of thyroid trapping only.
Use
- Detect hyperthyroidism
associated with low RAIU, e.g., factitious hyperthyroidism, subacute
thyroiditis, struma ovarii
- Evaluate use of
radioactive iodine therapy
- Determine presence of an
organification defect in thyroid hormone production
- T
suppression test. Administration of T causes less suppression
of RAIU in the hyperthyroid patient than in the normal person; has been
replaced by the TRH stimulation test.
Contraindications:
pregnancy, lactation, childhood.
Interferences
- Not valid for 2–4 wks
after administration of antithyroid drugs, thyroid hormone, or iodides;
the effect of organic iodine (e.g., radiographic contrast media) may
persist for a much longer time.
- Because of widespread
dietary use of iodine in the United States, RAIU should not
be used to evaluate euthyroid state.
- Increased by
- Withdrawal rebound
(thyroid hormones, propylthiouracil)
- Increased iodine
excretion (e.g., diuretic use, nephrotic syndrome, chronic diarrhea)
- Decreased iodine intake
(salt restriction, iodine deficiency)
Increased
(>12%) In
- Graves' disease (diffuse
toxic goiter)
- Plummer's disease (toxic
multinodular goiter)
- Toxic adenoma (uninodular
goiter)
- Thyroiditis (early
Hashimoto's disease; recovery stage of subacute thyroiditis)
- TSH excess
- TSH administration
- TSH production by
pituitary tumor (TSH >4 µU/mL) or other neoplasm
- Defective thyroid
hormone synthesis
- Thyrotropin-producing neoplasms
(e.g., choriocarcinoma, hydatidiform mole, embryonal carcinoma of testis)
Decreased
(<3%) In
- Hypothyroidism (tertiary,
secondary, late primary)
- Thyroiditis (late
Hashimoto's; active stage of subacute thyroiditis; RAIU does not usually
respond to TSH administration)
P.578
- Thyroid hormone
administration (T or T
- Therapeutic
- Factitious (RAIU is
augmented after TSH administration)*
- Antithyroid medication
- Iodine-induced
hyperthyroidism (Jod-Basedow)†
- Radiographic contrast
media, iodine-containing drugs, iodized salt
- Graves' disease with
iodine excess
- Ectopic hypersecreting
thyroid tissue
- Metastatic functioning
thyroid carcinoma*
- Struma ovarii*
- Use of certain drugs
(e.g., calcitonin, thyroglobulin, corticosteroids, dopamine)
Thyroxine
(T ), Free (Ft
See Table 13-3.
Use
- Gives corrected values in
patients in whom total T is altered because of
changes in serum proteins or in binding sites, e.g.,
- Pregnancy
- Drug use (e.g.,
androgens, estrogens, birth control pills, phenytoin [Dilantin])
- Altered levels of serum
proteins (e.g., nephrosis)
- Monitoring restoration to
normal range is only laboratory criterion to estimate appropriate
replacement dose of levothyroxine because 6–8 wks are required before TSH
reflects these changes.
Increased
In
- Hyperthyroidism
- Hypothyroidism treated
with T
- Euthyroid sick syndrome
- Occasional patients with
hydatidiform mole or choriocarcinoma with marked hCG elevations may show
increased FT , suppressed TSH, and
blunted TSH response to TRH stimulation. Values return to normal with
effective treatment of trophoblastic disease. Severe dehydration (may be
>6.0 ng/dL).
Decreased
In
- Hypothyroidism
- Hypothyroidism treated
with T
- Euthyroid sick syndrome
Thyroxine,
Total (T
See Tables 13-2 and , and Fig. 13-1.
Use
Diagnosis of hyperthyroidism
Increased
In
- Hyperthyroidism
- Pregnancy
- Drug effects (e.g.,
estrogens, birth control pills, d-thyroxine, thyroid extract, TSH,
amiodarone, heroin, methadone, amphetamines, some radiopaque substances
for radiographic studies [ipodate, iopanoic acid])
- Euthyroid sick syndrome
- Increase in TBG or
abnormal T -binding prealbumin
P.579
|

|
|
Table 13-4. Free Thyroxine Index in
Various Conditions
|
- Familial dysalbuminemic
hyperthyroxinemia—albumin binds T but not T more avidly than normal, causing changes similar to
thyrotoxicosis (total T ~20 µg/dL, normal
thyroid-hormone-binding ratio, increased FTI) but patient is not
clinically thyrotoxic.
- Serum T >20 µg/dL usually indicates true hyperthyroidism rather than
increased TBG.
- May be found in
euthyroid patients with increased serum TBG.
- Much higher in first 2
mos of life than in normal adults.
Decreased
In
- Hypothyroidism
- Hypoproteinemia (e.g.,
nephrosis, cirrhosis)
- Use of certain drugs
(phenytoin, T , testosterone, ACTH,
corticosteroids)
- Euthyroid sick syndrome
- Decrease in TBG
Normal
Levels May Be Found in Hyperthyroid Patients with
- T
thyrotoxicosis
- Factitious
hyperthyroidism due to T (Cytomel)
- Decreased binding
capacity due to hypoproteinemia or ingestion of certain drugs (e.g.,
phenytoin, salicylates)
Interferences
Various drugs
Not
Affected by
- Mercurial diuretics
- Nonthyroidal iodine
Thyroxine
Index, Free (Fti; T
- American Thyroid
Association now recommends the term thyroid
hormone–binding ratios (THBR).
- See Table
13-4.
Use
- This index is the
calculated product of T resin uptake and serum
total T . It permits correction
of misleading results of T and T
determinations caused by conditions that alter the T -binding
protein concentration (e.g., pregnancy, use of estrogens or birth control
pills).
P.580
Thyroxine-Binding
Globulin (Tbg)
Use
- Diagnosis of genetic or
idiopathic excess TBG
- Sometimes used for
detection of recurrent or metastatic differentiated thyroid carcinoma,
especially follicular type and cases in which patient has had an increased
level due to carcinoma.
- Differentiation of increased/decreased
total T or T
concentrations due to changes in TBG from normal free T
or T . Same purpose as T
resin uptake and FTI (see above).
Increased
In
- Pregnancy
- Use of certain drugs
(e.g., estrogens, birth control pills, perphenazine [Trilafon],
clofibrate, heroin, methadone)
- Estrogen-producing tumors
- Acute intermittent
porphyria
- Acute or chronic active
hepatitis
- Lymphocytic painless
subacute thyroiditis
- Neonates
Decreased
In
- Nephrosis and other
causes of marked hypoproteinemia such as liver disease, severe illness,
stress (T -binding-prealbumin also
decreased)
- Deficiency of TBG,
genetic or idiopathic
- Acromegaly (T -binding-prealbumin
also decreased)
- Severe acidosis
- Use of certain drugs
- Androgens, anabolic
steroids
- Glucocorticoids
(T4-binding-prealbumin is increased)
- Testosterone-producing
tumors
Decreased
Binding of T and T Due to Drugs
- Salicylates
- Phenytoin
- Tolbutamide (Orinase),
chlorpropamide (Diabinese)
- Penicillin, heparin,
barbital
- An
increased TBG is associated with increased serum T and
decreased T resin
uptake; a converse association exists for decreased TBG
Thyrotropin-Releasing
Hormone (TRH) Stimulation Test
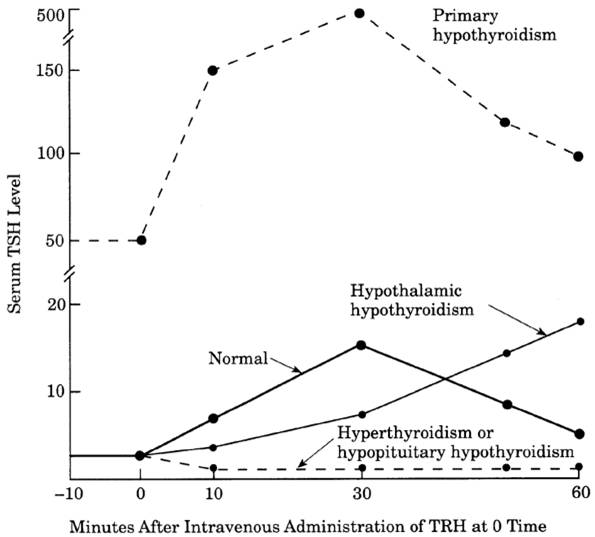
- See Fig.
13-2.
- Serum TSH is measured
before and 20 mins after IV administration of TRH (usually 500 or 200 µg).
- Normal response: a
significant rise from a basal level of ~1 µU/mL by 8 µU/mL at 20 mins and
return to normal by 120 mins. Response is usually greater in women than in
men.
- Primary hypothyroidism:
an exaggerated rise of an already increased TSH level
- Secondary (pituitary)
hypothyroidism: no rise in the decreased TSH level
- Hypothalamic
hypothyroidism: low serum T and T
and TSH levels, with a TRH response that may be exaggerated or normal or
(most characteristically) with a peak delay of 45–60 mins.
- Hyperthyroidism: TRH
administration does not cause a significant rise in serum TSH in
hyperthyroid patients as it does in normal persons; a normal rise (>2
µU/mL) virtually excludes hyperthyroidism. Absent response may also occur
in exophthalmic Graves' disease and nodular goiter.
P.581
|
|
|
Fig. 13-2. Sample curves of serum TSH
response to administration of thyrotropin-releasing hormone (TRH) in various
conditions.
|
- Blunted response may
occur in uremia, Cushing's syndrome, acromegaly, effect of certain drugs
(corticosteroids, levodopa, ‘large amounts of salicylates).
- Response may also be
suppressed in nonthyroidal conditions (e.g., starvation, renal failure,
elevated levels of glucocorticoids, depression, some elderly patients).
- The TSH response to TRH
is modified by T antithyroid drugs,
corticosteroids, estrogens, and levodopa. Response is increased during
pregnancy.
Use
- Interpretation must be
based on clinical studies that exclude the pituitary gland as the site of
the disease.
- Now largely replaced by
TSH.
- Confirmation of
hyperthyroidism when other test results are equivocal. Lack of response
shows adequate therapy in patients receiving thyroid hormones to shrink
thyroid nodules and goiters and during long-term treatment of thyroid
carcinoma.
- Differentiation of two
forms (whether or not due to tumor) of thyrotropin-induced hyperthyroidism
- May be particularly
useful in T toxicosis cases in which
the other tests are normal or in patients clinically suspected of
hyperthyroidism with borderline serum T levels. TRH stimulation
test is superior to the T suppression test of
RAIU. Abnormal TSH response to TRH administration does not definitely
establish the diagnosis of hyperthyroidism (because autonomous production
of normal or slightly increased amounts of thyroid hormones causes
pituitary suppression). TRH test may remain abnormal even after successful
therapy of Graves' disease.
- Hyperthyroid patients in
whom associated nonthyroid conditions result in only slight elevation of
serum T and T
- Euthyroid Graves' disease
patients presenting with only exophthalmos (unilateral or bilateral). TRH stimulation test may sometimes be normal in these
patients, and T suppression test may be required
- Elderly patients with or
without symptoms of hyperthyroidism may have serum T
and T in upper normal range.
P.582
- Euthyroid sick syndrome.
Generally serum TSH is normal with a relatively normal TSH response to
TRH.
- May help differentiate
hypothalamic from pituitary hypothyroidism (see previous section)
|
|
Baseline TSH (µU/mL)
|
Change in TSH 30 Mins after TRH
Administration (µU/mL)
|
|
Euthyroidism
|
<10
|
>2 (95% of cases)
|
|
Hyperthyroidism
|
<10
|
<2
|
|
Primary hypothyroidism
|
>10
|
>2 (exaggerated)
|
|
Secondary hypothyroidism
|
<10
|
<2
|
|
Tertiary hypothyroidism
|
<10
|
>2 (delayed or exaggerated or
normal)
|
|
Triiodothyronine
(T
See Table 13-3 and Fig. 13-1.
Use
- Diagnosing T
thyrotoxicosis (TSH is suppressed but T is normal) or cases in
which FT is normal in presence of
symptoms of hyperthyroidism
- Evaluating cases in which
FT is borderline elevated
- Evaluating cases in which
overlooking diagnosis of hyperthyroidism is very undesirable (e.g.,
unexplained atrial fibrillation)
- Monitoring the course of
hyperthyroidism
- Monitoring T
replacement therapy—is better than T or FT4 but TSH is
preferred to both.
- Predicting outcome of
antithyroid drug therapy in patients with Graves' disease
- Evaluating
amiodarone-induced thyrotoxicosis
- Serum T
parallels FT4; is early indicator of hyperthyroidism but TSH is better.
- Good biochemical
indicator of severity of thyrotoxicity in hyperthyroidism
- Not recommended for
diagnosis of hypothyroidism; decreased values have minimal clinical
significance.
- May decrease by
≤25% in healthy older persons, whereas FT4 remains normal.
- Free T
gives corrected values in patients in whom the total T
is altered because of changes in serum proteins or in binding sites, e.g.,
- Pregnancy
- Drugs (e.g., androgens,
estrogens, birth control pills, phenytoin)
- Altered levels of serum
proteins (e.g., nephrosis)
Triiodothyronine
(T ) Resin Uptake
See Table 13-4.
Use
- Measures unoccupied
binding sites on TBG. Is not a measure of T
- Only with simultaneous
measurement of serum T to calculate T
to exclude the possibility that an increased T
is due to an increase in T4-binding globulin. Measurement of serum T
concentration should be done by RIA for diagnosis of hyperthyroidism.
Increased
In
See causes of decreased
serum TBG.
Decreased
In
See causes of increased
serum TBG.
Normal In
- Pregnancy with
hyperthyroidism
- Nontoxic goiter
- Carcinoma of thyroid
P.583
- Diabetes mellitus
- Addison's disease
- Anxiety
- Use of certain drugs
(e.g., mercurials, iodine)
Variable
In
Liver disease
Diseases
of the Thyroid
See Table 13-3.
Carcinoma
of Thyroid
- Medullary carcinoma
- Sporadic (noninherited)
accounts for 80% of cases
- Familial accounts for
20% of cases
- MEN type I.
- Most are MEN type II.
- Familial non-MEN.
- Basal serum calcitonin may be increased in patients with medullary carcinoma
of the thyroid.
- Serum Tg levels are increased in most patients with differentiated thyroid
carcinoma but not in undifferentiated or medullary carcinoma. May not be
increased with small occult differentiated carcinoma. May be useful to
detect presence and possibly extent of residual, recurrent, or metastatic
differentiated carcinoma. Increased levels may be
found in patients with nontoxic nodular goiter; presence of autoantibodies
interferes with the test.
- Serum CEA may be
increased in medullary carcinoma and may correlate with tumor size or
extent of disease.
- Serum LD, CEA, and Tg
may be increased in advanced follicular carcinoma.
- Serum T3, T4, and TSH
are almost always normal in untreated patients. Rarely, evidence of
hyperthyroidism may be found with large masses of follicular carcinoma.
- Laboratory findings due
to associated lesions (e.g., pheochromocytoma and parathyroid tumors) (10–20% of cases of medullary carcinoma of thyroid occur as
part of MEN) and due to production of additional substances (e.g.,
ACTH, serotonin, histaminase) by medullary carcinoma
- RAIU is almost always
normal.
- Radioactive scan of
thyroid
- Needle biopsy of thyroid nodule
Euthyroid
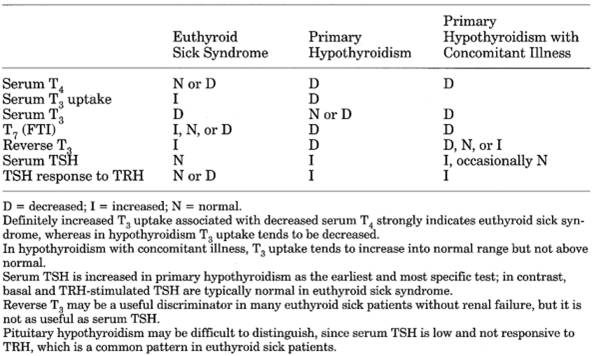
Sick Syndrome (Nonthyroidal Illness)
- (Wide
variety of nonthyroidal acute and chronic conditions such as infection,
liver disease, cancer, starvation, renal failure, heart failure, severe
burns, trauma, and surgery may be associated with abnormal thyroid
function tests in euthyroid patients, especially in aged persons;
artifactual changes in thyroid tests are not included in euthyroid sick
syndrome.)
- No
single test is clearly diagnostic, especially in elderly and acutely or
severely ill patients
- See Table
13-5.
- Initial change in all
nonthyroidal illness patients is decreased T
with increased rT . With increasing
severity, serum T declines, producing low
T –low T state.
- Increased
T
syndrome is most common (≤20%) in acute psychiatric admissions,
especially in the presence of certain drugs (e.g., amphetamines,
phencyclidine) and in old age (≤15% of elderly patients); increased
values tend to decrease during first 2 wks after admission as patient
improves. Is rarer in acutely ill patients (e.g., those with acute
hepatitis).
- Increased serum T , FTI, and T
- TSH is usually normal in
mild to moderate illness.
P.584
|
|
|
Table 13-5. Differential Diagnosis of
Euthyroid Sick Syndrome
|
- TRH test often is not
useful due to flat TSH response commonly seen in melancholia patients.
- 50% of patients with
hyperemesis gravidarum show elevated total and sometimes free T that persist until hyperemesis abates. Patients with symptomatic
hyponatremia show transient increase until low sodium is corrected.
- Decreased
T
Syndrome
- Occurs in >50% of
patients with severe or chronic illness.
- TSH is transiently
increased (few days or weeks) during recovery.
- Low T
syndrome is the most common. Occurs in most illnesses, starvation, and
after surgery or trauma. T is decreased in ~70% of
hospitalized patients without intrinsic thyroid disease and is normal in
20–30% of hypothyroid patients; therefore T
testing is not indicated.
- Increased rT
- With progressive
illness, tendency is for fall in total T and TBG with increase of free T4. Thus T uptake increases, and FTI tend to remain normal. A strong
correlation is seen between low T (<3 µg/dL) and high
mortality in hospitalized patients.
- Serum TSH is typically
normal or slightly increased; TSH response to TRH is usually normal.
In
Neonates
- Occurs in ~2.5% of
newborns, particularly in association with prematurity, obstetrical or
neonatal stress or illness, postmaturity.
- Decreased serum T4.
- Decreased serum T3.
- Normal serum TSH.
- By age of 1 mo, serum T is normal in 98% of these infants.
- By age of 4 mos, if T is still decreased, two-thirds of cases are due to genetic TBG
deficiency.
Goiter,
Neonatal
Due To
- Maternal ingestion of
iodine (e.g., for thyroid disease, for asthma), propylthiouracil
- Inherited hypothyroidism
(diminished ability to synthesize thyroid hormones)
- Neonatal hyperthyroidism
P.585
- Dyshormonogenesis
- Hemangioma, lymphangioma